Cardiac Ejection Fraction
Understanding Cardiac Ejection Fraction
The term “Cardiac Ejection Fraction” (EF) is a critical parameter in the realm of cardiology, offering insights into the heart’s pumping efficiency. Specifically, EF measures the percentage of blood that is ejected from the left ventricle with each heartbeat. This value is essential for diagnosing and managing various heart conditions, as it reflects the heart’s ability to supply the body with sufficient blood. Typically, a normal ejection fraction ranges from 50% to 70%, indicating that the heart is functioning well. Values below this range may suggest heart conditions such as heart failure or cardiomyopathy, while values above it could indicate hypertrophic cardiomyopathy.
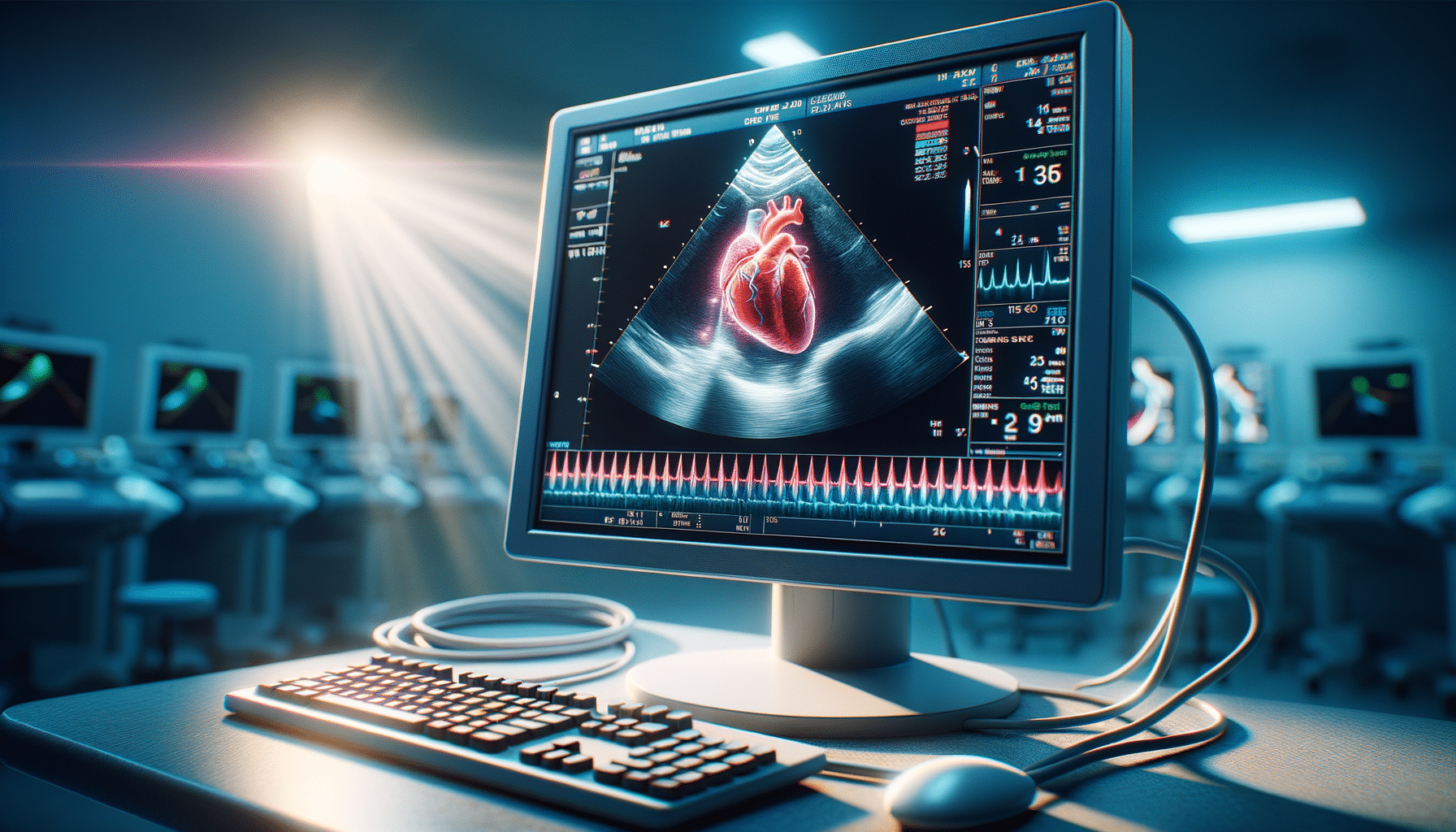
Healthcare professionals often use imaging techniques like echocardiograms, magnetic resonance imaging (MRI), or nuclear medicine scans to assess EF. These tools provide visual evidence of heart function, allowing for precise measurement of the ejection fraction. Understanding EF is crucial for both patients and healthcare providers, as it plays a key role in determining treatment strategies and monitoring the progression of heart disease.
The Role of Ejection Fraction in Diagnosing Heart Conditions
The cardiac ejection fraction serves as a pivotal diagnostic tool in identifying various heart conditions. A reduced EF is often associated with heart failure, a condition characterized by the heart’s inability to pump blood efficiently. This can lead to symptoms such as fatigue, shortness of breath, and fluid retention. Conversely, an elevated EF might suggest hypertrophic cardiomyopathy, where the heart muscle thickens and impairs its function.
In clinical practice, EF is not just a standalone measure but a part of a comprehensive assessment that includes patient symptoms, medical history, and other diagnostic tests. For instance, in cases of heart failure with reduced ejection fraction (HFrEF), patients may be prescribed medications to improve heart function and reduce symptoms. Monitoring EF over time helps healthcare providers adjust treatment plans and evaluate the effectiveness of interventions.
Moreover, EF values are instrumental in stratifying patients for advanced therapies such as implantable devices or surgical interventions. In summary, the measurement of EF is indispensable in the diagnostic and therapeutic landscape of cardiology.
Imaging Techniques for Measuring Ejection Fraction
Accurate measurement of cardiac ejection fraction is paramount, and several imaging techniques are employed to achieve this. The most common method is echocardiography, which uses ultrasound waves to create images of the heart. This non-invasive procedure provides a clear view of the heart’s chambers and valves, allowing for precise calculation of EF.
Magnetic Resonance Imaging (MRI) is another highly effective tool for assessing EF. It offers detailed images and is particularly useful when echocardiography results are inconclusive. MRI can provide comprehensive insights into cardiac structure and function, making it a valuable resource in complex cases.
Nuclear medicine scans, such as the multigated acquisition (MUGA) scan, are also utilized to evaluate EF. These scans involve the use of radioactive tracers to visualize blood flow through the heart, offering yet another perspective on heart function. Each of these techniques has its advantages and limitations, and the choice of method often depends on the specific clinical context and patient needs.
Interpreting Ejection Fraction Results
Interpreting ejection fraction results requires a nuanced understanding of cardiac physiology and individual patient circumstances. A normal EF (50%-70%) generally indicates healthy heart function, while values below this range suggest varying degrees of heart dysfunction. For instance, an EF of 40%-49% may indicate mild heart failure, whereas an EF below 40% suggests more severe heart failure.
On the other hand, an EF above 70% could point to hypertrophic cardiomyopathy, a condition where the heart muscle becomes abnormally thick. It’s important to note that EF is just one piece of the puzzle; other factors such as symptoms, medical history, and additional tests are crucial for a comprehensive diagnosis.
Healthcare providers must consider the entire clinical picture when evaluating EF results. For example, a patient with a low EF but minimal symptoms might require a different treatment approach compared to someone with similar EF but severe symptoms. The goal is to tailor interventions to optimize heart function and improve quality of life.
Advancements in Ejection Fraction Measurement
Recent advancements in technology have significantly improved the accuracy and ease of measuring cardiac ejection fraction. Innovations in imaging techniques, such as three-dimensional echocardiography and cardiac MRI, provide more detailed and precise assessments of heart function. These advancements enable earlier detection of heart conditions and more personalized treatment plans.
Moreover, the integration of artificial intelligence (AI) in imaging analysis is revolutionizing the field. AI algorithms can quickly and accurately interpret complex data, assisting healthcare providers in making informed decisions. This technology not only enhances diagnostic accuracy but also reduces the time required to analyze results.
Looking forward, continued research and technological advancements hold promise for further improving the assessment of ejection fraction. These developments will likely lead to better patient outcomes and more efficient healthcare delivery. As the field evolves, staying informed about these changes is crucial for both healthcare providers and patients.